Although I am a doctor, I don’t always see the progress
Redaktor "Głosu Fizjoterapeuty"
Ireneusz Orman, 53 years old comorbidities: hypothyroidism, chronic kidney disease, status post three episodes of phlebitis
On the 16th of April I was on call in the hospital (I am a gynecologist) when suddenly felt my temperature rise. I managed to get myself a test on the next day but I had to wait three days for the results. At first there was no fever, I just started feeling weaker. On Monday it turned out that I was infected. My temperature began to rise. When I started experiencing shortness of breath after a week, my daughter drove me to the hospital. I was given some medications in the department of pulmonology and my condition seemed to improve. However, I suffered from serious dyspnea overnight and they had to take me to the ICU and connect to OptiFlow. My condition was defined as critical but stable. Nonetheless, I wasn’t really improving much and the damage to my lungs was progressing – which is why they decided to intubate me. The next five days I know only from stories, because I slept through them all. I know I went into septic shock in the meantime and my inflammation markers rose almost to the upper laboratory detection limits. Fortunately, my condition was managed by plasmapheresis. After several days I developed renal failure and had to undergo dialysis. Upon recovery from anaesthesia, I had to stay in the ICU for the next week.
Mobilization from the beginning
My physiotherapy has already started in the ICU. One day after recovering from anaesthesia I had my first postural drainage. Standing up was still impossible because my saturation would instantly drop when I tried sitting. Verticalization was successful only after a few days. During that week there were days when I felt really awful and wasn’t able to do much – but I exercised every day. When I was transferred to the department of pulmonology, I attempted walking in place for the first time. I feared that my muscles had gotten really weak after spending so many days in bed. So it really calmed me down when a physiotherapist checked my muscles and reassured me that things weren’t as bad as I expected. It was quite uplifting. I managed to take a short walk around the room after two weeks from the day when I recovered from anaesthesia. Since I was still very weak, I was forbidden from walking around the room unassisted but I could move along the windowsill, as the window was close to my bed.
The damage to my lungs was so serious that I was advised to lay on my stomach for two hours every day. At first, when I still had a urinary catheter and ECG electrodes attached to my chest, it was a bit inconvenient. But now I don’t find this position uncomfortable anymore.
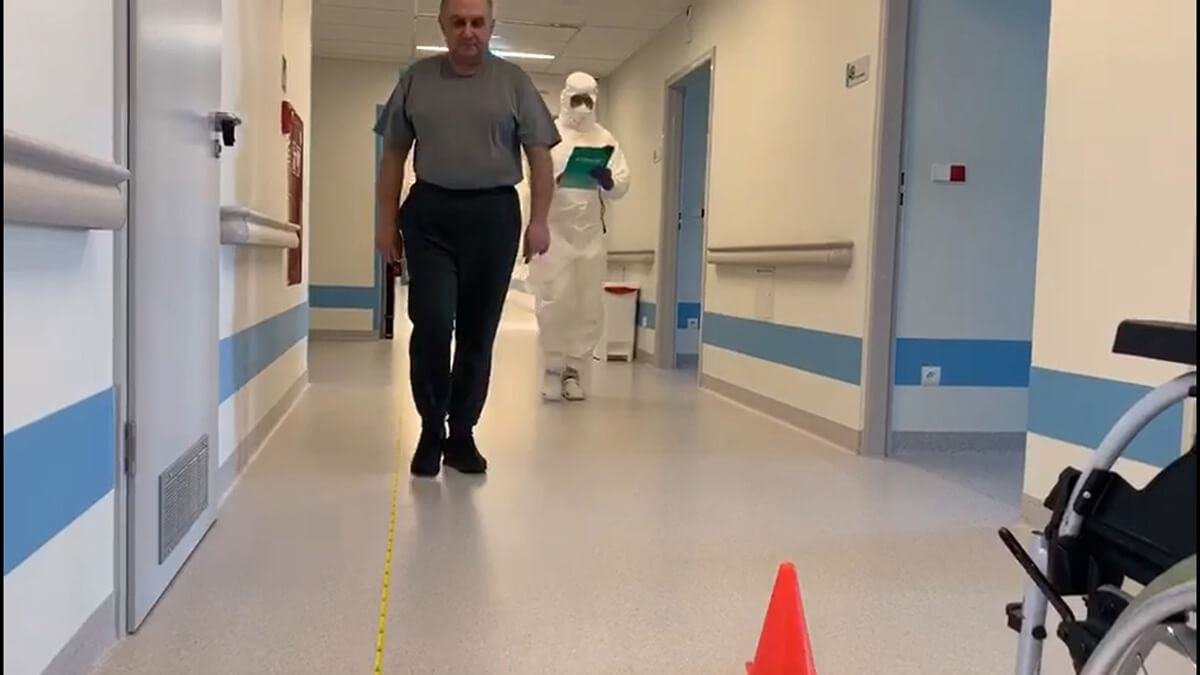
I made a large progress when I could first walk the hall. At first, I was able to walk 7.5 meters, of course with small breaks and constant saturation control. Physiotherapy lasted for about an hour at that time. Then it prolonged to 2 hours as I became able to walk 15 m. After spending a month in hospital, I was finally able to take a shower – that was something!
Support of physiotherapist
It is incredibly important that I was visited by someone who lifted my spirits up. Who ensured me that I was going to manage, motivated me and noticed progress which I was sometimes unable to see, even though I am a doctor. But he could see it when he looked at me. He payed attention to such small details. This psychological aspect is incredibly important. With such long stays in hospital – and I have been here for a month and a half now – some depressive tendencies start to appear. I am not given a lot of medications here so I guess the primary reason why I’m here is the process of improving my functionality during physiotherapy sessions. We work for two hours, from Monday to Friday. I am now able to walk without holding onto objects, I just need some assistance.
I think that they discharge me home as soon as a negative test result comes. I can take care of myself but I am also aware of my limitations and I know have to take things one at a time. I am still not sure how my treatment is going to look when I leave the hospital, whether I will have to come for follow-ups. Anyway, I feel I am still going to need physiotherapy and a specialist to direct my activities. Considering my recent experiences, I am know feeling quite well, I have regained the ability to take care of myself. But the road to full recovery and regaining my physical condition from before the disease is still very long.
Daj znać, co sądzisz o tym artykule :)
Redaktor "Głosu Fizjoterapeuty"