Redaktor "Głosu Fizjoterapeuty"

 +3
+3 Refraining from rehabilitation is like asking for complications
Refraining from rehabilitation is like asking for complications
Refraining from rehabilitation is like asking for complications
Refraining from rehabilitation is like asking for complications
Refraining from rehabilitation is like asking for complications
Refraining from rehabilitation is like asking for complications
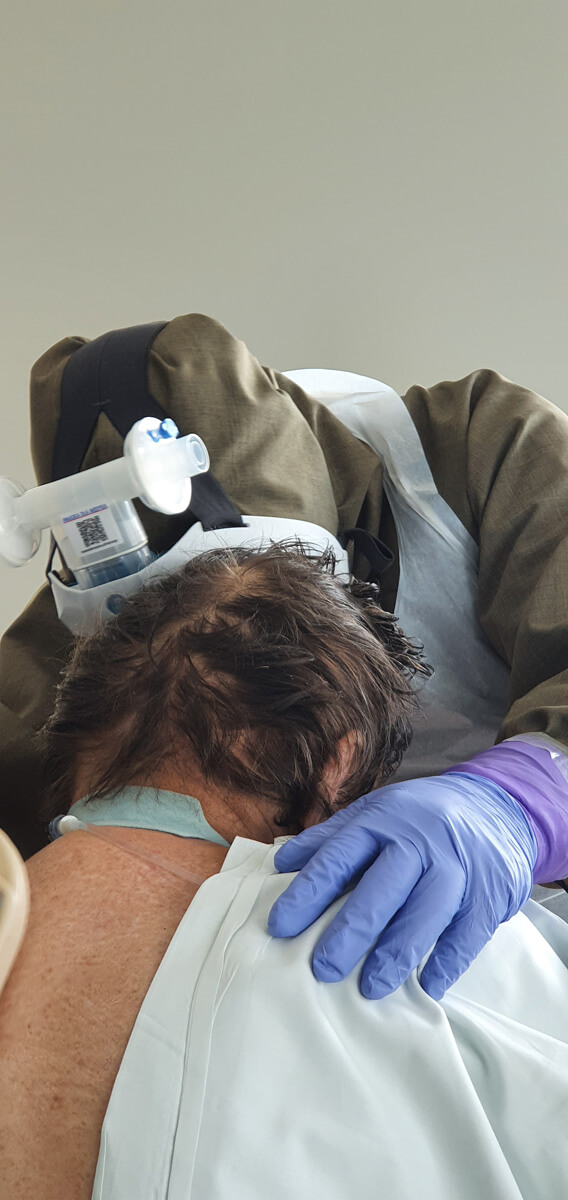
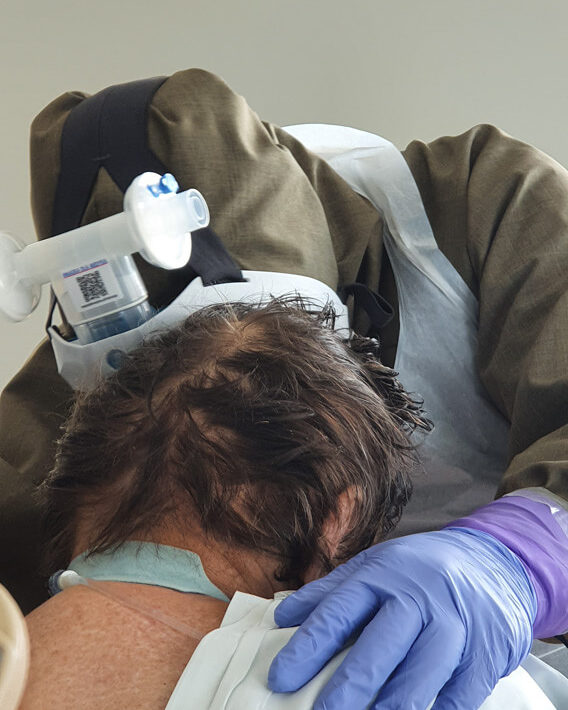
“Physiotherapy for COVID-19 patients must be introduced from the very beginning. They might recover without it but not necessarily regain their physical fitness from before the disease” – we read about cooperation with physiotherapists, as told by Konstanty Szułdrzyński MD, PhD, internal medicine and anaesthesiology specialist, chief of the Center of Extracorporeal Therapies at the University Hospital in Cracow, now transformed into an infectious diseases hospital.

Konstanty Szułdrzyński, MD, PhD – Internal medicine and anaesthesiology specialist, chief of the Center of Extracorporeal Therapies at the University Hospital in Cracow, now transformed to an infectious diseases hospital.
Agnieszka Gierczak-Cywińska: Why is the presence of physiotherapists essential in your department?
Konstanty Szułdrzyński: Our department has been created six months ago, by combining two other departments from different locations. Physiotherapists have been here from the very beginning, working in 5-6 workplace positions. I really appreciate our cooperation. There are two aspects which I find particularly important. First of all, our patients do not stay on our ward longer than it is necessary, since they are immediately mobilized and therefore can leave the ward faster. Second of all, it often seems that a patient who is lying down is in a relatively good condition. But the true verification of his well-being takes place during exercise tests, when he is asked to perform certain activities. The experience of physiotherapists is incredibly valuable here. Sometimes doctors state that a patient’s condition hasn’t changed and then a physiotherapist tells us that this patient has in fact improved because today he can do something that he wasn’t able to do before or he tolerates bigger effort. Furthermore, I think that exercises have a very good influence on the emotional state of patients. Thanks to physical activity, they can see that their treatment is going in the right direction.
They start noticing small progress?
Exactly. Patients are unable to interpret information from various monitoring machines, but they sure can see if their physical condition improves. And this can be very uplifting. This can motivate you to fight for your health.
When compared to doctors, physiotherapists spend more time with the patients, which can give them a lot of support – especially now, when family visits in hospitals are not allowed.
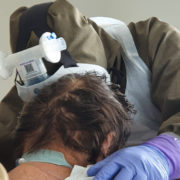
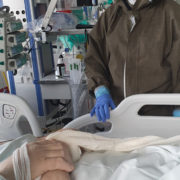
We all know that nurses are the ones who spend the most time with patients, after them are physiotherapists. Doctors are present during visits and, if nothing happens later, there is no need for them to come. But this live contact between two people is absolutely crucial. Especially now. Even when the circumstances for a casual conversation are not very favourable, because the patient is intubated- they are still able to establish some form of contact with them.
When do you introduce physiotherapy for COVID patients?
From the very beginning. It is possible even in deep analgosedation or during muscular relaxation. Moving patients in such conditions provides them with adequate tromboprophylaxis, enables lymphatic drainage, allows to maintain mobility of joints, prevents contractures and has many other benefits. Of course physiotherapy cannot be performed on unstable patients but when there are no clear contraindications – patients are being rehabilitated from the very beginning.
Is five or six a sufficient number of physiotherapists on your ward?
Definitely not. In the ICUs in the United States there are as many physiotherapists as there are nurses. Sessions with stronger patients might really take a lot of time, while weaker patients have shorter sessions which are repeated several times a day. Obviously the progress is much faster under such circumstances, but what can we do? Let’s appreciate whatever help we get.
How long do patients diagnosed with coronavirus stay in your hospital?
If there are no complications, patients usually spend the first week on a normal ward. Then the condition of some patients deteriorates very rapidly, so they may end up in our unit for another week, then come back on the regular ward and stay there for another week or two. But if serious complications occur, patients might lie on our ward for weeks.
How is it possible that a patient, who has been in hospital for a week, suddenly deteriorates to such an extent that he/she has to be transferred to the ICU?
We don’t know that, this disease has a very unpredictable course.
What was the maximum amount of COVID patients that you had on your ward? And how many are there now?
The biggest number was 20, maybe 22. Now (29th of May – editorial note) there are seven.
So is the pandemic calming down?
That’s what it seems right now. However, we’re starting to admit more patients from the Silesia region, some of which are in a critical condition. When they run out of available beds, they start sending patients to us, since it’s really close from Katowice. Another reason is that we perform ECMO (extracorporeal membrane oxygenation) and no other hospital in this region is able to offer such a treatment.
Do many patients require ECMO?
No, I would even say that it’s a surprisingly small amount of cases. If patients receive appropriate mechanical ventilation and are not disturbed, their condition improves relatively fast. Unless we’re talking about very old patients or the ones who have numerous comorbidities. We haven’t observed any deaths due to respiratory failure in the ICU. There were always some other reasons, such us circulatory failure. They have always improved in terms of respiratory function.
Is physiotherapy necessary for COVID-19 patients?
Physiotherapy allows patients to regain their physical health and shortens their stay in the ICU. If a patient stays longer in the ICU and then is transferred to a regular ward without having regained some functionality, it is very likely that he/she will stay longer on this regular ward. And the longer he/she stays there, the bigger the risk for complications. There may be other infections, pulmonary embolism, thrombosis and thousands of other unexpected episodes. Refraining from rehabilitation is like asking for complications.
Patients are rehabilitated in the ICU, then on the regular ward. What’s next?
It is very important that especially elderly patients, those who leave hospital in worse overall condition or those whose stay in the hospital was longer, receive referral to some rehabilitation facility, where they can be admitted to a day ward and well taken care of. But such things are in a dramatic condition in this country, even without COVID-19. There is not one public facility like that in Cracow. We used to send some patients to Limanowa or even to Otwock. From Cracow! Polish healthcare system focuses only on eliminating the primary diagnosis. If somebody used to have pneumonia and now no longer has pneumonia – he/ she is considered healthy. And the fact that this patient lies in bed, is unable to work, requires assistance in simple daily activities – nobody cares about that.
Do you think it happens due to lack of knowledge, lack of intuition, insufficient funds?
Everything at once. It all begins from our attitude towards quality in medicine. Please note that the only parameter which is not evaluated in the Polish healthcare system is the quality of treatment. A patient’s condition when he or she is discharged from hospital has no influence on the institution’s funding. But if a hospital’s funding was dependant on patients’ condition when they are discharged, instead of on the sole fact of whether they left hospital or not – then it would become profitable for healthcare institutions to take better care of their patients’ condition. Another problem is this unfortunate Polish system, where NFZ and ZUS function as separate entities even in terms of disability pensions. If NFZ was obliged to pay disability pensions, it would be in its best interest to allow patients regain full functionality as quickly as possible as it would make NFZ stop paying disability pensions and save money. Moreover, this healthy individual would happily go back to work and continue paying health insurance contributions.
Physiotherapists are alarming that they are still underappreciated by doctors and hospital directors.
That makes us go back to the aspect of quality in healthcare. If quality was a priority, every hospital director would do their best to hire more physiotherapists, because that would allow patients to regain functionality much faster. No doctor, nurse or dietician is able to complete this task – only a physiotherapist is capable of restoring a patient’s physical fitness. But if NFZ pays the same amount of money for patients who leave hospital on their own, as well as for patients who are carried out of the hospital on stretchers – then what is the point in hiring physiotherapists, from the perspective of hospital directors? Polish physiotherapy is very similar to dentistry – it is almost completely privatized. Whoever can afford it – pays for maintaining good physical condition. Unfortunately, the majority of people can’t afford it. Especially those, who need such a help the most. As a results, we end up with a society which has an incredibly low percentage of working people, as some are too old and others benefit from earlier retirements or disability pensions.
And how are you holding up mentally after almost three months of very intensive work?
It has been quite alright but it’s probably due to the fact that we’ve admitted a relatively small number of patients in such a large hospital, where our department benefits from latest technologies and is well equipped. Of course I am exhausted by not having at least two days off work for the past three months, since I work shifts – 12 hours at work, 24 hours off and again 12 hours at work etc. In the long run, it’s really tiring. There are less COVID patients than before but they still appear. Some of them improve very slowly and stay in our unit for long periods of time. And if we get someone in a very serious condition, just like the patient that is now connected to ECMO, he might give us a month of sleepless nights.
Daj znać, co sądzisz o tym artykule :)
Redaktor "Głosu Fizjoterapeuty"